Unconventional Applications in Dental 3D Printing

About the author
Dr. Andrew Ip is a Sydney-based private general dentist and speaker/educator on dental 3D printing technologies. As a clinician, he provides many treatments, including complex crowns and bridges, braces, and implants. Some of his academic achievements include a Graduate Diploma in Orthodontics and a Masters of Science in Implantology and Dental Surgery. He is currently undergoing a Graduate Diploma in Digital Dentistry.
The AI3D-Dentiq provisional – a novel two-piece 3D printed screw-retained provisional implant restoration
The digitization of dentistry has unlocked many potential applications in modern clinical and technical practice. It is clear that 3D printing is becoming an increasingly popular and effective part of that equation. Gone are the days where it seemed like you needed a PhD to operate a 3D printer. Chairside dental 3D printing has become extremely cost-effective and simple-to-learn with many dental-specific systems known to be highly consistent, accurate, precise and reliable.
Dental technology has allowed us to create excellent provisional restorations, cost-effective dentures, same-day or even same-appoint nightguards, and more! However the beauty of 3D printing is that applications are only limited by your imagination, restrictions placed in design software, and the materials currently available in the market. It gives the clinician and technician the opportunity to let their creativity run rampant, all while improving the patient experience.

Pre Op
A 65-year old male attended our practice with a severely broken upper right first premolar (#14) that had been designated to be extracted a number of years ago. The tooth immediately distal (#15) was also in need of substantial dental treatment. He had hypertension that was controlled with anti-hypertensive medication but was otherwise medically fit. He had intentions to improve the colour of his current anterior teeth but wished to address the issues on his upper right side first.


Tooth #14 was deemed unrestorable and so it was decided to extract the tooth, wait for bony healing and replace it with an implant with a provisional restoration. During the healing process, endodontic therapy would be performed on tooth #15. Following bony integration, #14 would be restored with a screw-retained direct-to-fixture zirconia crown and #15 would also be restored with a full-coverage zirconia crown. A deliberately lighter shade would be chosen, factoring in the patient’s long-term desire to improve the colour of his existing teeth.
Implant Planning
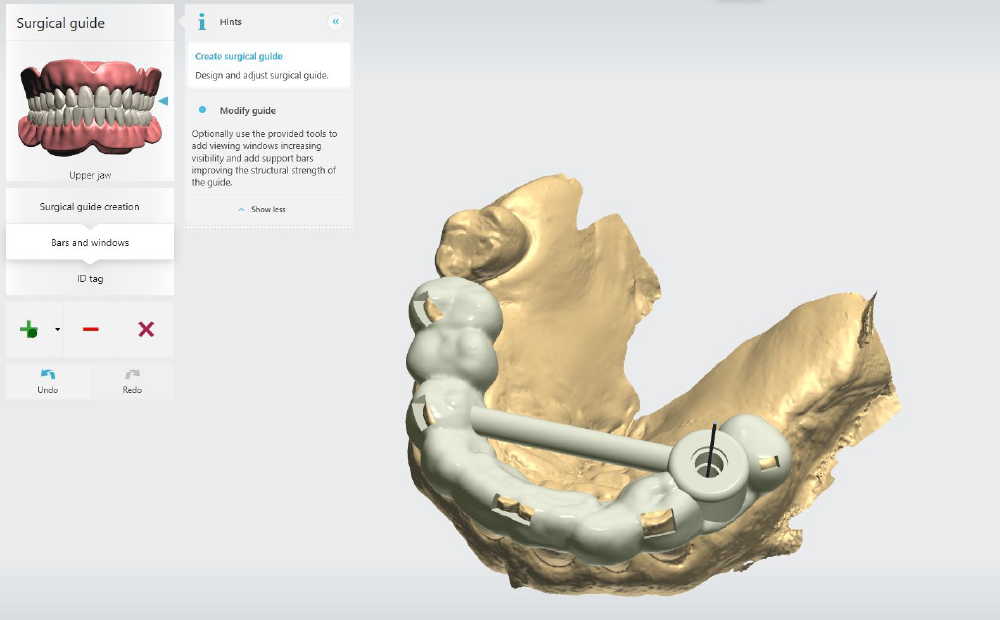
2 months after #14 was extracted, a CBCT scan (NewTom GO) and intraoral scan (Medit 1700w) were performed and the two datasets were merged on 3Shape Implant Studio in order to plan the patient’s case. Implant planning and surgical guide design was Jeroen Klijinsma of Dentiq Dental Services. The use of surgical guides has been shown to enhance accuracy and precision in many users(1).
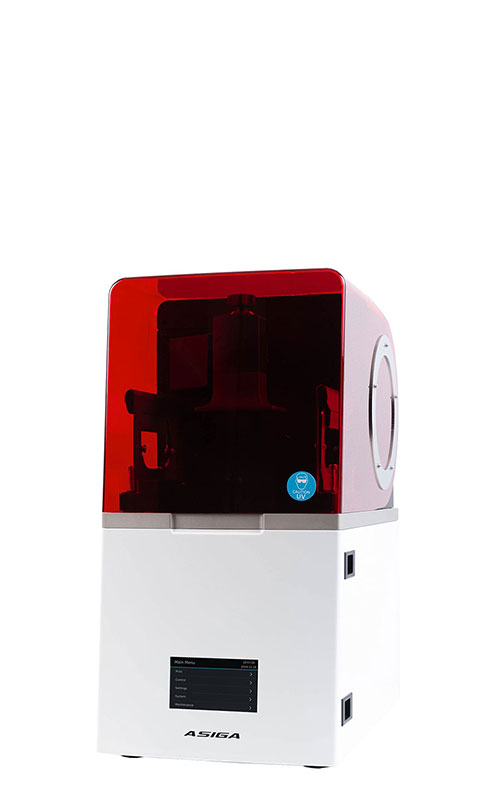
A Tri Matrix 4.1×8.0mm tissue-level fixture was digitally positioned in order to design the surgical guide, based on parameters already pre-loaded on the extensive 3Shape Implant Studio library. A pilot guide was designed in this case as it has been shown to produce similarly accurate results in comparison to fully guided systems(2). The surgical guide was printed out of Voco Surgical Guide resin on the Asiga Max UV at 50 micron layers and was autoclaved after complete processing.
Provisional Restoration Design
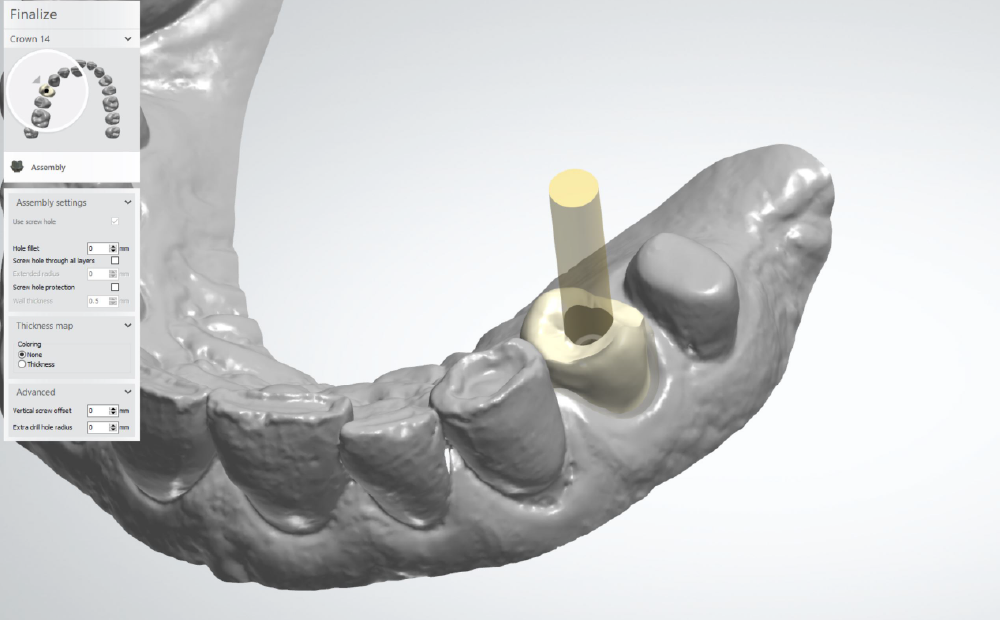
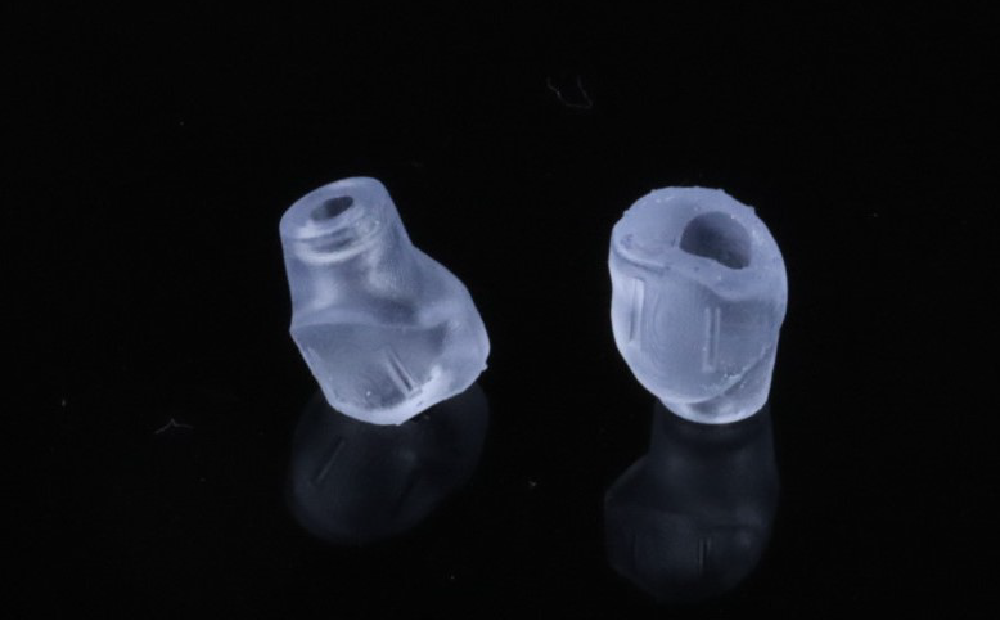
Based on the implant plan, a two-piece provisional restoration was designed using the same software. The abutment portion provisional would be printed in a clear splint material (Keysplint Hard) which would be highly polished for optimum transparency. This would allow visibility of the healing process. To reduce the amount of polishing required, the abutment would be printed:
- At 50 micron layers to reduce the appearance of layer lines
- Using the Asiga UltraGLOSS™ material tray
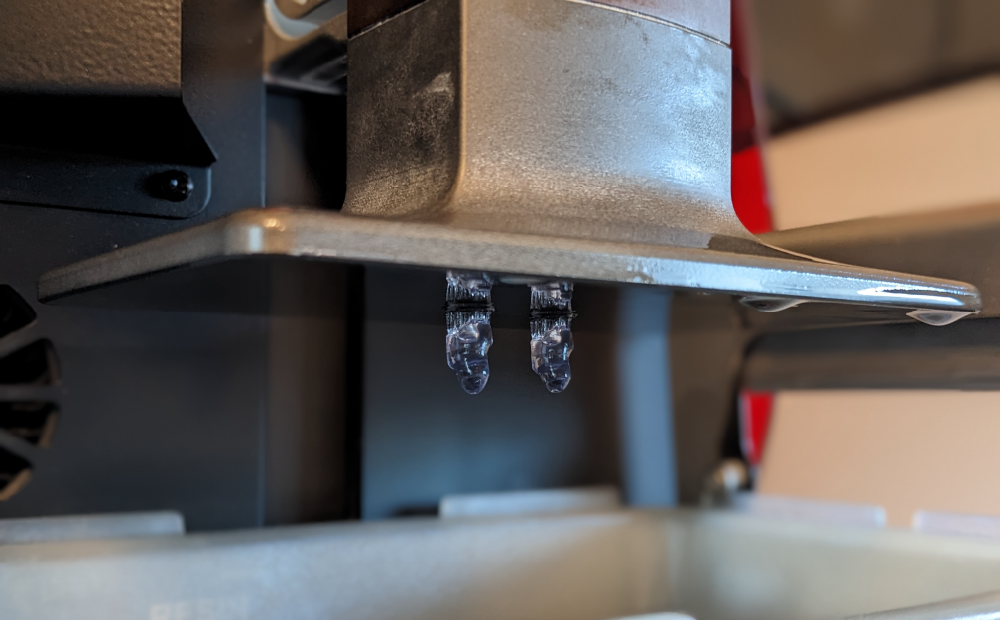
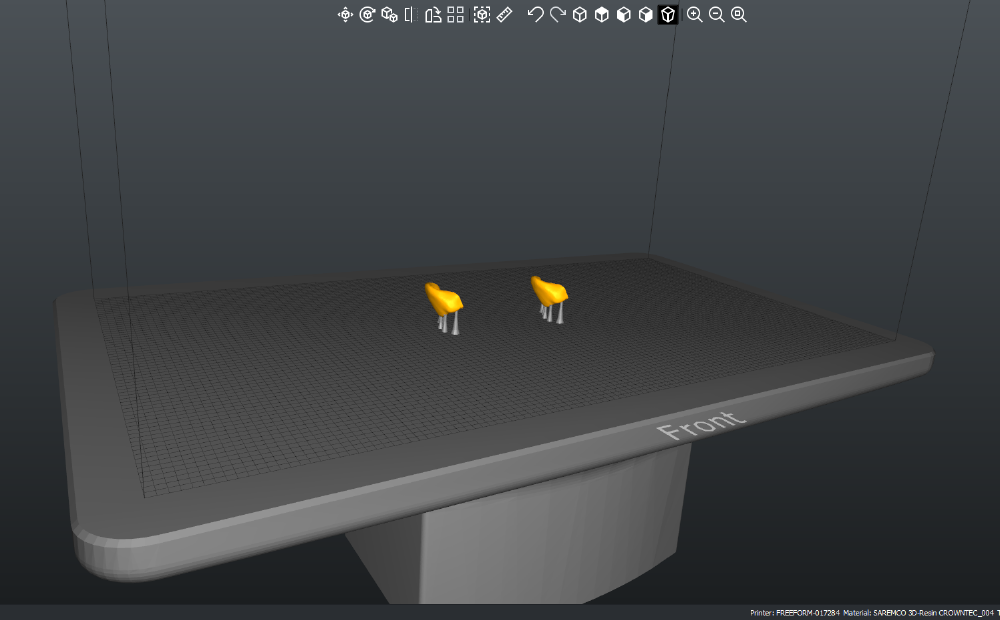
Printing the temporary abutments out of Keysplint Hard on the Asiga Max UV using the UltraGLOSS™ material tray
A separate facial veneer would be bonded to this abutment and would be printed in a restorative resin (Saremco Crowntec) to satisfy the aesthetic concerns of the patient. 2 retentive slots would be incorporated on to the abutment and veneer to ensure proper fixation during the bonding process.
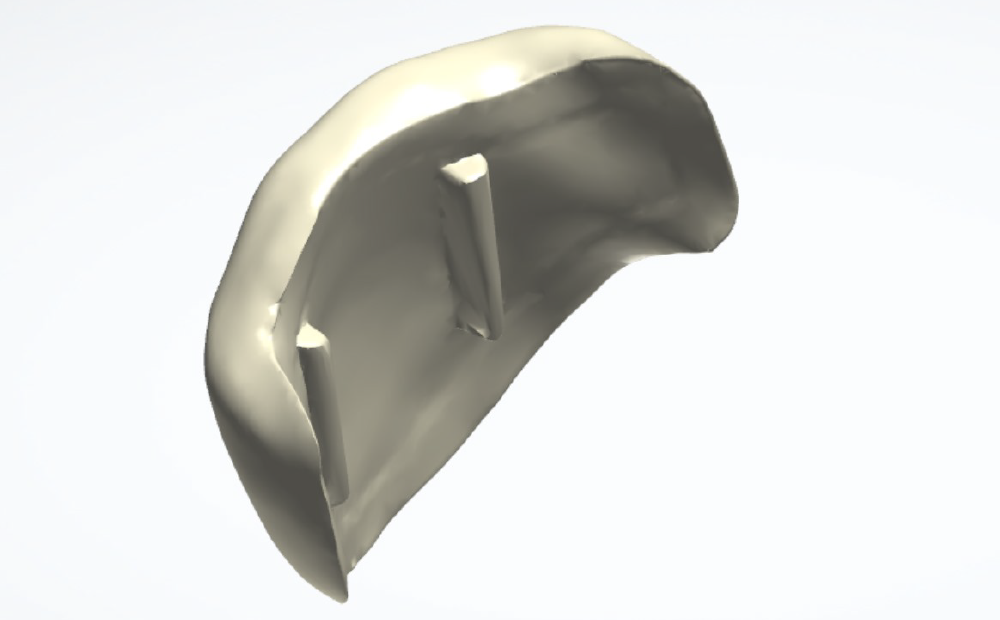
Veneer – facial aspect
Veneer – fitting surface
Veneers nested and supported on Asiga Composer 2.0
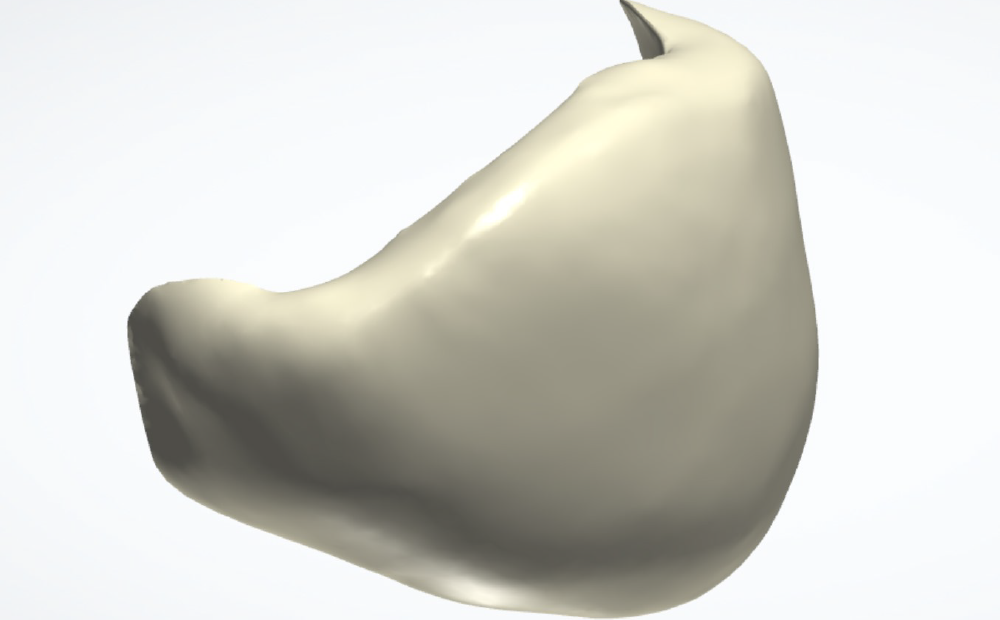
Prior to final cure on the Otoflash (2x 2000 flashes), the two pieces would be bonded together using the splint resin as a cementing agent.

One should mention that what makes this all possible is the novel and innovative Tri Matrix implant connection, which lacks any sharp corners/edges, allowing for direct-to-fixture milled and printed restorations.


Implant placement and provisionalisation
The fit of the surgical guide was confirmed and the patient was anaesthetised locally.
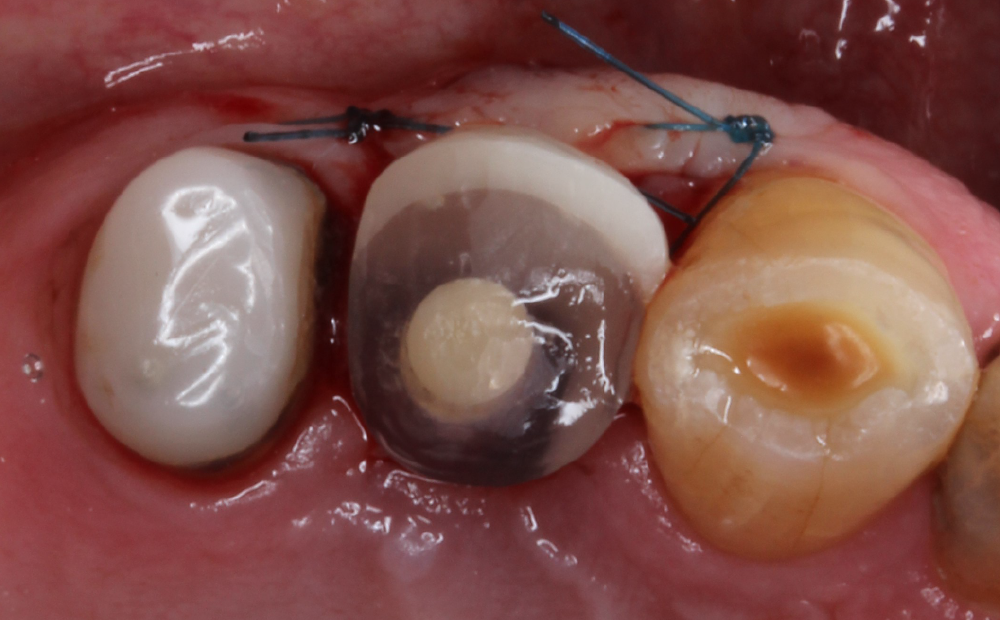
A small full-thickness flap was raised and a guided osteotomy was performed. A Tri Matrix 4.1×8.0mm implant was inserted at 45Ncm torque. The pre-fabricated two-piece provisional was torqued in at 15Ncm and was confirmed to be out of occlusion. Two Prolene 4-0 sutures were used to close the flap.
Suture removal occurred 14 days later and the patient reported uneventful post-operative healing at this stage. Endodontic therapy was commenced on tooth #15 in the meantime.
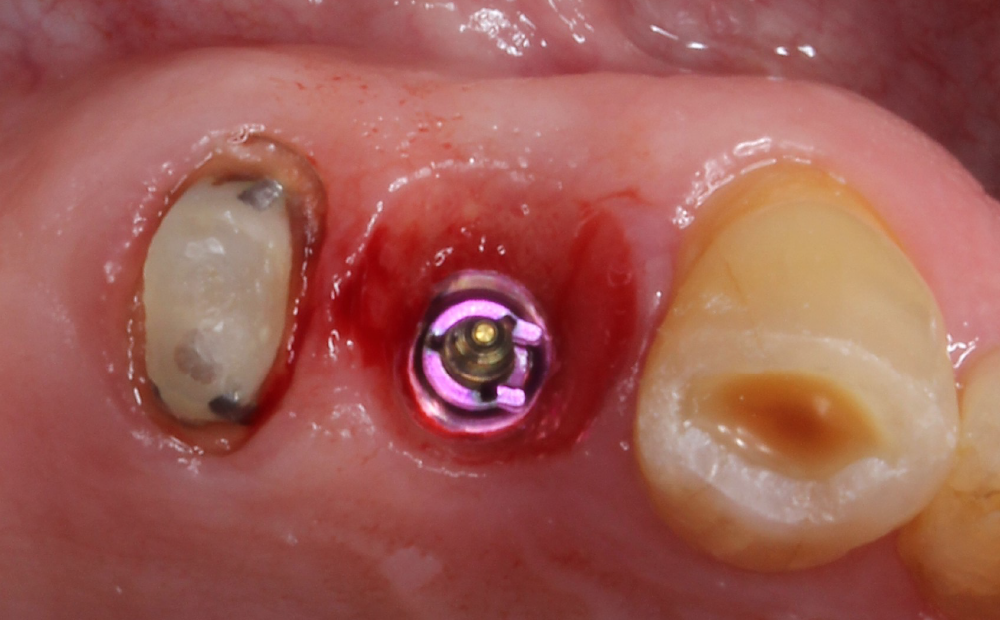
Immediate situation post-surgery
Immediate situation post-surgery occlusal perspective

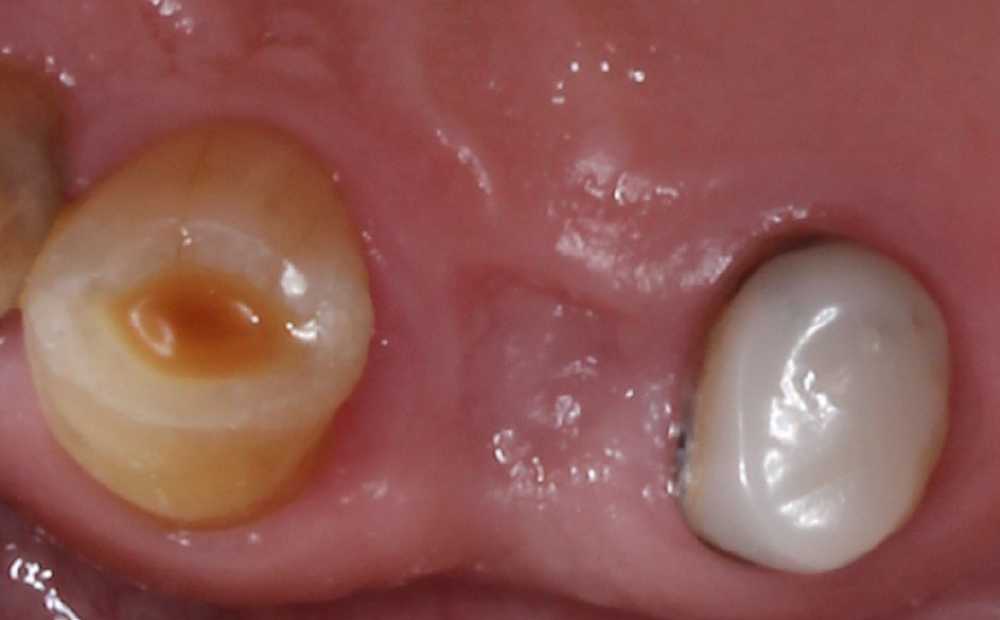
Implant and tooth restoration
A waiting period of four months allowed adequate osseointegration of the implant.

The endodontic treatment of tooth #15 had been completed in the meantime and it had been prepared for a full-coverage zirconia crown. Removal of the implant provisional restoration revealed a natural soft tissue profile and an improved soft tissue contour without the need for additional soft and/or hard tissue augmentation.
A secondary impression was taken digitally with an intraoral scanner and the relevant scan body. Definitive restorations were designed on Exocad and milled in-house on the DOF Craft-5X out of UNC Everest AT multilayer zirconia (shade A3). A deliberately lighter shade was chosen by the patient as he had intentions to improve the appearance of his other remaining upper teeth. The implant crown was torqued in at 35Ncm and the #15 crown was cemented using G-Cem One cement.


Conclusion
Digital dentistry and novel techniques can help produce excellent and effective results. Improvements in the software and physical workflow has meant that the clinician’s and the technician’s experiences are not only more streamlined and straightforward, but also enjoyable. A more-than-satisfactory outcome was achieved with the patient. Overall 3D printing and software can unlock numerous applications to not only improve patient outcomes, but also the operator experience. It will be truly exciting to see the innovations that lie ahead.
References:
- Scherer U, Stoetzer M, Ruecker M, Gellrich NC, von See C. Template-guided vs. non-guided drilling in site preparation of dental implants. Clin Oral Investig. 2015 Jul;19(6):1339-46.
- Kühl S, Zürcher S, Mahid T, Müller-Gerbl M, Filippi A, Cattin P. Accuracy of full guided vs. half-guided implant surgery. Clin Oral Implants Res. 2013 Jul;24(7):763-9
Share: