A game changer for chairside splint production.
Case study written by Dr Kasen Somana, Principal Dentist, Signature Dentistry, Australia.
From their inception, porcelain laminate veneers have become a staple in modern cosmetic practice. Their indications include the corrections of tooth shape and position, closing of diastemas and masking tooth discoloration. In terms of aesthetics and tooth conservation, these restorations have been proven to be incredibly successful1,2.
When enhancing or rejuvenating a smile, the key is to achieve minimal tooth reduction. The conservative nature of veneer preparation allows for ultra-thin veneers that can be relatively fragile. With advances in material sciences, we now have numerous porcelains with improved aesthetics, bond strength and fracture toughness3. These materials allow the dentist to conservatively design smiles and favorably direct functional forces. However, when nonfunctional forces are applied, as in the case in bruxism, long-term success can be affected.
Bruxism can complicate porcelain veneer prognosis, hence in some clinical situations, porcelain veneers may be contraindicated4,5. According to the American Academy of Orofacial Pain, bruxism is a diurnal or nocturnal parafunctional activity which includes clenching, bracing, gnashing and grinding of the teeth6. It is defined as a forcible clenching or grinding of the teeth, or a combination of both in non-functional movement of the jaw.
Magne et al. reported that failure rates increased in the presence of uncontrolled bruxism. Managing bruxism in the form of a nocturnal and/or diurnal splint is recommended as a preventative measure to reduce the risk of failure7,8. Occlusal splints allow the mandible to continue the nonfunctional excursive movements whilst balancing the force distribution across the arch, thus protecting the veneers.
Case study.
A 34-year-old female presented with aesthetic concerns. She found her smile to be unflattering and wanted to improve her overall aesthetics and self-esteem. She wanted slightly sharper “feline” upper canines and a whiter smile.
Treatment Plan:
After thorough co-diagnostic digital smile design and planning, the patient decided on 10 porcelain veneers and 2 resin veneers. The increased length of her upper canines presented a potential risk for increased lateral forces in excursive movements. In addition, the patient reported a history of bruxism.
Occlusal Splint Design & Material:
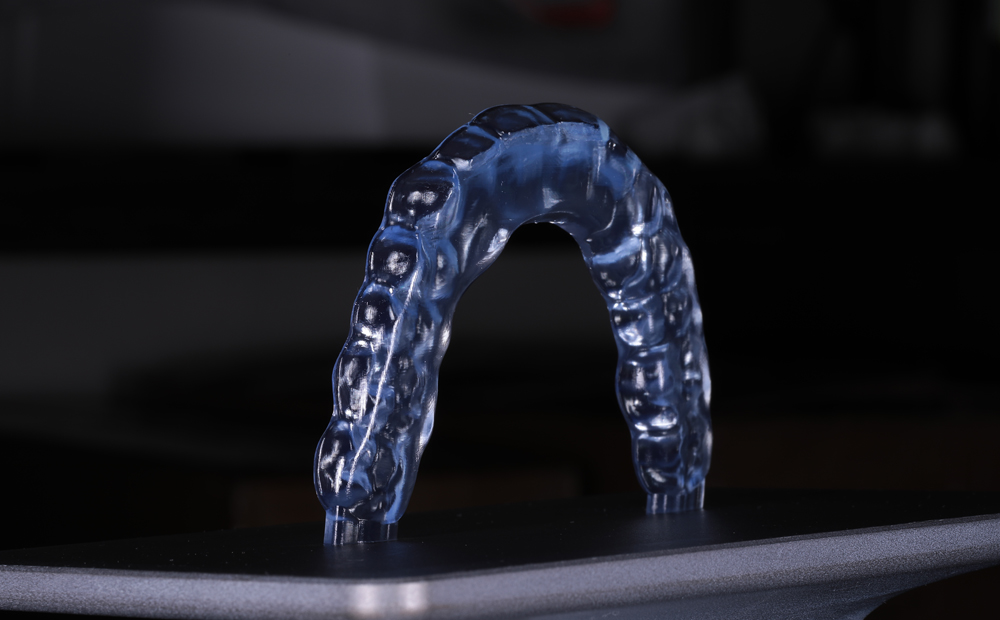
Flat plane occlusal splint was decided as ideal and the scans were sent for Ai Design via 3Shape Design Services. This is a 15-minute design service enabling same day productions.
Material: Keyprint KeySplint Soft
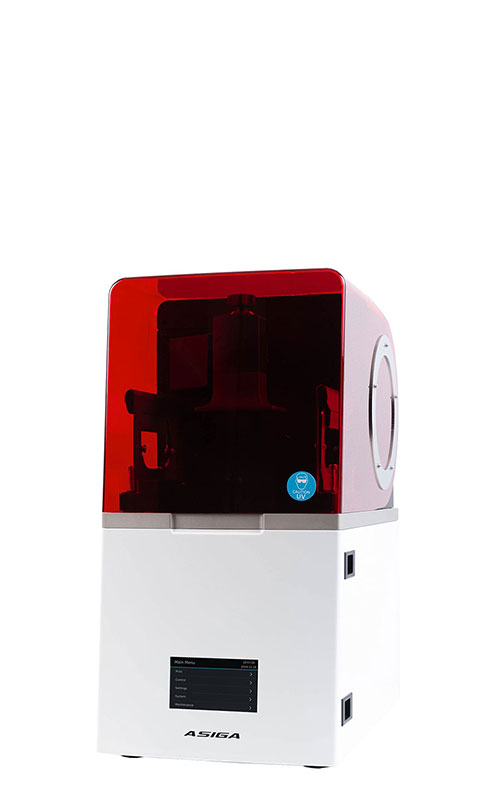
3D Printer:
Asiga Max UV with UltraGLOSS™ material tray and Composer 2.0 software.


Occlusal Splint Fit:
The printed occlusal splint had an incredibly accurate fit with little discomfort or noticeable pressure on the anterior teeth. Due to the digital design process and digital bite registration, only minor occlusal adjustment was required.


Benefits of the Asiga UltraGLOSS™ material tray:
The post processing time had been all but eliminated. Apart from the standard washing and post curing requirements, trimming off the sprues at the distal saddle of the splint was the only manual labor required. This allowed us the flexibility of manufacturing and delivering a perfect occlusal splint within a day.
KeySplint soft has always had a high patient compliance due to the fit and nature of the material. Now with the release of the UltraGLOSS™ material tray, chairside fabrication has become effortless and time efficient without compromise.
Conclusions:
Longevity of restorations (in the absence of debonding or fracture) is quintessential in successful clinical practice. Patients with bruxism exhibit a three times higher probability of debonding and eight times higher probability of porcelain fractures compared to their non-bruxing counterparts. As such, the use of occlusal splints reduces the failure rate of porcelain laminate veneers in patients with bruxism. Having the ability to provide a same day design and production service with nominal manual labour has now become my gold standard treatment. In addition, the KeySplint material and the accuracy of 3Shape Design service consistently produces exceptionally comfortable occlusal splints which increase patient compliance and in turn increase the longevity of dental restorations.


Tips and Tricks for Printing:
- Thoroughly mix your KeySplint resin prior to pouring into the UltraGLOSS™ material tray
- If you already have KeySplint resin in the UltraGLOSS™ material tray, it may be good practice to always clean your build tray according to the Asiga Protocol by exposing the tray to 30 seconds of UV light. Then peel off the cured resin for the base prior to mixing the resin in the tray.
- When designing your splint, add an extra 3mm of solid form to the distal portion on the splint. This will establish a stable anchor for the splint when mounting it on the build platform. For consistent results, place the splint at a 9-degree angle as shown in Figure 1.
- Double check that you are using the UltraGLOSS™ material tray profile in Asiga Composer and print at the receommended layer thickness of 50-microns.
- After printing, use 2 baths with fresh 99% IPA solution. The first bath is to remove the bulk of uncured resin and the second bath is for a thorough wash for 5 mins.
- After washing and air drying, place the splint in an oxygen free environment and cure for the recommended curing times (times are specific to curing chamber manufacturer).
- Once cured, remove the distal extension portion with an acrylic bur and lightly buff the area. You are now ready to issue the high gloss splint.
About Dr Kasen Somana
BSc Hons (Melb) BDS Hons (Syd) MSc (Lond) MFGDP (UK)

Dr Kasen Somana has been in private practice in Melbourne, Australia for almost 20 years and is the principal dentist of Signature Dentistry in Toorak. His practice has a special interest in conservative digital aesthetic fixed prosthodontics and occlusal rehabilitation. Determined to provide the highest level of care to his patients, he often participates and lectures at digital dental conferences locally and internationally. He is a key opinion leader for 3Shape and Asiga.
References:
- Chen W, Raigrodski AJ. A conservative approach for treating young adult patients with porcelain laminate veneers. J Esthet Restor Dent. 2008;20:223-238.
- Fons-Font A, Solá-Ruiz MF, Granell-Ruiz M, Labaig-Rueda C, Martínez-González A. A choice of ceramic for use in treatments with porcelain laminate veneers. Med Oral Patol Oral Cir Bucal. 2006;11:e297-302.
- Freire A, Archegas LR. Porcelain laminate veneer on a highly dis- coloured tooth: a case report. J Can Dent Assoc. 2010;76:a126.
- Walls AWG. The use of adhesively retained all-porcelain veneers during the management of fractured and worn anterior teeth: Part 2. Clinical result after five years follow-up. Br Dent J. 1995;178:337- 340.
- Peumans M, Van Meerbeeck B, Yoshida Y, Lambrechts P, Van- herle G. Five-year clinical performance of porcelain veneers. Quin- tessence Int. 1998;29:211-221.
- American Academy of Orofacial Pain. Okeson JP, ed. Orofacial Pain. Guidelines for assessment, diagnosis, and management. Chi- cago: Quintessence Publish Co; 1996. p. 49-73.
- Magne P, Perroud R, Hodges JS, Belser UC. Clinical performance of novel-design porcelain veneers for the recovery of coronal volume and length. Int J Periodontics Restorative Dent. 2000;20:440-57.
- Christensen GJ, Christensen RP. Clinical observations of porcelain veneers: a three-year report. J Esthet Dent. 1991;3:174-9.
Share: